Returning to Work- COVID-19 Precautions and Protections
by Six Month Smiles, on 7/6/20 11:49 AM
The COVID-19 pandemic has imposed unprecedented restrictions on how we practice dentistry and many of you are trying to figure out how to provide a safe environment for your staff and customers. The American Dental Association has complied an excellent set of resources in a booklet titled “Return to Work Interim Guidance Toolkit.” If you haven’t done so, please download it from HERE. This toolkit has checklists, protection strategies, screening guidelines, and so on.
While the toolkit is full of processes and procedures, we thought to also compile practical tips from the collective wisdom of some of “forward leaning” dentists, who have been in operations for a while. Here are some of the things they have shared with us.
Efficiency:
Overall, the biggest challenge dentists face is efficiency. Cleaning the operatory between patients and not going between operatories (to limit cross-contamination) severely limits how many patients can be seen during a typical workday. The number we hear is that dentists are allowing about 30 minutes of extra time per patient visit.
Patient Management & Screening:
The waiting area is closed. Patients have to wait in their vehicles and call the front office for someone to get them. Follow ADA guidelines on patient screening. Patients respond favorably to this as they understand that the procedures are for their protection.
Visuals:
Establish traffic flows and markers. Use arrows and stickers to mark direction of traffic and social distance markers to indicate what’s 6 feet apart.
Ambient:
The research shows that the COVID-19 virus becomes non-pathogenic in a few minutes under bring sunlight. If your operatories allow, let in natural sunlight, and open windows to let in fresh air.
Ventilation, Filtration and Disinfection of Ambient Air:
Enhancing ventilation and cleaning the ambient air helps patients and staff feel more comfortable. Options range from low-tech (open windows), to proven (HEPA filtration), to exotic read “dubious” (Ozone disinfection).
Open Windows:
Undeniably, opening windows to let in fresh air will reduce the ambient viral load but it’s a very low-tech approach that’s not controllable and will result in excessive temperature and humidity swings.
HEPA Filters:
There is ample body of evidence to suggest that HEPA filters offer good protection by removing viral particles. While the virus itself is too small to filter, they are carried around in water droplets, that can be filtered. If you are considering investing in HEPA filtration, do note that you must ensure that the air is directed from the source (patient) to the HEPA filter. This is better achieved with a portable HEPA devices than HEPA filtration for your central air-conditioning system. Portable units work well, are visible to the patient, but can be noisy. Also note that if you have multiple units running, a harmonic noise can set up, that rises and falls in intensity, think a dull police siren. To minimize this possibility, invest in the biggest HEPA portable filter system and run it at lower speeds or at different speeds. Consumer Reports has a good article on HEPA filters, that you can access HERE.
Ozone (Airborne):
Ozone is a very powerful decontaminant but, based on OSHA guidelines, is toxic. Breathing in ozone can result in shortness of breath, wheezing, and coughing. OSHA limits concentration of ozone in air to 0.1 ppm, which is far lower than the gaseous concentration required to kill airborne pathogens. Despite these warnings, vendors are selling ozone “air purifiers.” DO NOT fall for this scam and stay away from ozone generators.
Disinfection of Aerosolized Water:
Using treated water in your dental equipment offers the possibility of self-disinfection, that is, during an aerosol producing procedure, the aerosolized water droplets would be rendered harmless by dissolved chemical/gas, protecting you, your staff and your office from contamination. There are two options for treating water: dissolved ozone or dissolved chlorine.
Ozone (in water):
Ozonating the water used in your chair can disinfect capabilities but with the caveat that there are no reliable studies that support its use in dental equipment. Aqueous ozone has a very short shelf-life so it must be generated on-site and then used within a few minutes. Given this limitation combined with the risk of a malfunctioning ozone generator, aqueous ozone is not widely used. There is a dearth of published literature on safe concentrations of aqueous ozone for human consumption but from what we can gather, ozone concentration of 8-10 ppm is reportedly safe to drink yet 1 to 3 ppm of aqueous ozone with a contact time of 4-10 minutes can kill waterborne pathogens. On paper, aqueous ozone works but chlorine, below, is a far better and proven alternative.
Chlorine (in water): Like ozone, chlorine is a toxic gas but when dissolved in water, chlorine (aka bleach) offers very effective disinfection with a much longer shelf-life than aqueous ozone. Chlorine is also inexpensive and is widely used as a disinfectant for drinking water. In the United States, municipalities are regulated to deliver a certain concentration on chlorine in tap water. Measuring chlorine in your water source is also easy and reliable using inexpensive water test kits. Per the CDC, concentrations of only 1 ppm (or less) inactivate a majority of virus in under a few minutes and chlorine concentration of up to 4 or even 5 ppm is safe for human consumption. Furthermore, limited exposure at higher levels, up to 10 ppm is OK. Its not uncommon to find such high levels of chlorine in swimming pools and spas.
If you are in the United States, there is a good chance that the residual chlorine in your tap water is already over 1 ppm. This would be great news because your source water already offers a certain level of self-disinfection if its aerosolized. To boost the level of chlorine in your source water, you can add a small quantity of household bleach. Regular household bleach ranges from 5.25%~8% NaChl, which translates to 50,000 – 80,000 ppm available chlorine therefore, a 1000:1 dilution will yield 5-8 ppm of chlorine in your source water. Since chlorine is well-regulated and studied, compared with aqueous ozone, there is less risk of a liability issue. As an additional benefit, if you can maintain high levels of chlorine, you can discontinue the use of shock tablets and straws. Chlorine in your equipment line will control biofilm.
Lastly, and most importantly, CONSULT YOUR DENTAL CHAIR MANUFACTURER BEFORE PROCEEDING WITH CHLORINE DOSING. CHLORINE IS CORROSIVE, DEGRADES POLYMERS (ORINGS/TUBING), AND MAY VOID YOUR WARRANTIES.
PPE:
Opinions on PPE vary, and your regulatory body may stipulate minimum PPE requirements. The ADA toolkit has some commonsense recommendations, such as wearing long sleeve clothes, discarding disposable gowns after each use, and changing out of scrubs upon entry and exit. There is a lot of latitude in level of PPE that the ADA is recommending and what you and your staff need to implement to be safe and comfortable. Highlighted below is feedback from our dentists.
Face Mask and Shields:
N95 masks are becoming more widely available and cost anywhere from $1 to $4 apiece. Some of you chose to wear the mask all day while others only during an aerosol producing procedure. If availability is limited, consider wearing level 1 or level 3 over the N95 to avoid it getting soiled.
Alternately, we have heard rave reviews for Miakomo face masks because they are flexible, comfortable that can be reused (disinfect and sterilize). Reportedly, you can cut 4 or 5 filter elements from one N95 mask for your Miakomo. Check them out HERE.
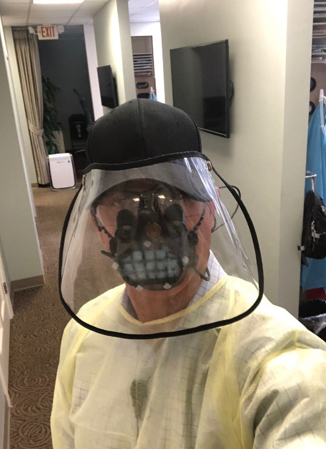
Opinions are mixed on face shields. Doctors do wear them particularly when they are doing an aerosol procedure. Otherwise, the face shields tend to fog up but this hack of using a baseball cap seems to work to hold up the face shield.
Gowns and Scrubs:
Some doctors are wearing protective head covers (see above photo), scrubs over scrubs and shoe covers throughout the day, while others only wear scrubs for all procedures except when producing aerosols. Then the doctors wear N95 mask and face shields.





